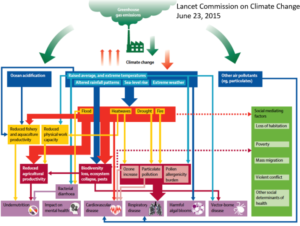
A consequence of the rapid, often complex changes taking place in patterns of disease and risk is a widening gap between population needs and the capacity of health systems to meet these. This is reflected in many countries’ weak performance tackling the Millennium Development Goals. Societal aging and lifestyle changes bring growing need for promotive and preventive strategies; little is known about ways to strengthen social support systems.
Such changes in disease burden and population structure, and greater opportunity to reshape health systems, accentuate the need for longitudinal, comparative research to inform strategy.
Objectives, questions and hypotheses
This working group will investigate the implications of epi-demographic change for health and welfare systems, including changes in disease profiles, population structure, utilisation of services and population ageing. The studies will:
- Evaluate the performance of local services against MDG targets using HDSS data on maternal, child and adult mortality, including deaths from HIV/AIDS, tuberculosis and malaria
- Examine how best to
- extend HDSS sites to function as health and health system “observatories” monitoring health status, access to and use of services, and health system responses in a standardised way
- modify health systems – and evaluate the effects on population health – to support a continuum of care across the life-course including more integrated primary health care for chronic illness
- strengthen support systems for older persons and evaluate the effects on their wellbeing.
Looking ahead, we hypothesise that introducing point-of-care diagnostics and hand-held electronic data capture will shift primary care from clinic to community settings; this will improve access to curative and health-promoting interventions, resulting in better health outcomes.
Methods and analyses
HDSS data
Work will involve site-specific and comparative epi-demographic and contextual analyses of HDSS and health systems data, taking account of the effect of migration on denominators. This will permit evaluation of changes in: proportions of children / older persons; age-sex profiles of mortality and probable cause-of-death; fertility trends; and the influence of household socioeconomic status on these measures. From this, we can evaluate progress in meeting MDG targets among rural and urban populations, and contribute data to statistical offices; where progress is off-target, we will highlight some steps necessary to improve this.
Record linkage
Variable use of services means that clinic or hospital-based surveillance is prone to a biased presentation of population health needs. A critical opportunity exists to link patient records (from clinics, district hospitals) and surveillance systems. Through such ‘linkage’, disease or risk in residents can be related to their use of services, supporting analyses of patterns of access, utilisation and service coverage. Questions relate to usage by socioeconomic status and systematic shortfalls in coverage of marginal communities. INDEPTH centres provide a test-bed for approaches to record linkage whether based on matching algorithms, digital fingerprinting or photo-IDs. INESS experience will contribute important insights as linkage is necessary to support multi-centre therapeutic trials and post-administration surveillance; linkage carries real potential for service improvement.
Key deliverables
Policy-relevant findings will help assess progress against MDGs; effects of epidemics on health systems; and consequences of population change for communities and social services. Findings will inform trials of complex interventions e.g. integrated chronic care or support for older persons. We expect to demonstrate the role of health system “observatories” as sources of evidence on the performance of front-line health systems; and strengthen capacity to apply data on health outcomes to evaluations of health system performance.
The working group has developed two big projects:

 Call us:(+233)0244806015
Call us:(+233)0244806015  Email
Email